
17 . 05 . 2019
Sleep Deprivation and Alzheimer's Disease
The restorative effect of sleep has deserved great scientific attention in recent years. Poor sleep in quantity and quality increases the risk of cardiovascular disease, cancer, and dementia. This article will focus on the influence of sleep deprivation on the development of dementia, specifically Alzheimer’s disease.
Dementia is a growing problem in the aging population of industrialized countries, with Alzheimer’s disease accounting for about 60-80% of cases. The latter is a significant cause of mortality and morbidity, affecting the quality of life of patients and their families.
What is Alzheimer’s disease?
Alzheimer’s disease is a neurodegenerative disorder that leads to a gradual deterioration of memory initially, and executive functions at a later stage. The diagnosis is most common after age 65 and patients live on average eight years after diagnosis.
What is the mechanism of neuronal injury in Alzheimer’s disease?
Today, Alzheimer’s disease is recognized as a multifactorial entity in which different mechanisms contribute to the dysfunction and premature death of neurons. Histologically, the hallmark lesions of this disease are amyloid plaques and neurofibrillary tangles.
Amyloid plaques are aggregates of β-amyloid protein which is a product of neuronal metabolism. The exact function of the amyloid protein in the brain is still debated, with some evidence that it may have antimicrobial activity and its production being increased when there is inflammation.
Neurofibrillary tangles are composed of hyperphosphorylated tau protein. Tau protein has a stabilizing effect of the neuronal microtubules and is fundamental for its correct functioning. However, when hyperphosphorylated by enzymatic reactions, it aggregates into filamentous structures that constitute the neurofibrillary tangles, which interfere with neuronal function.
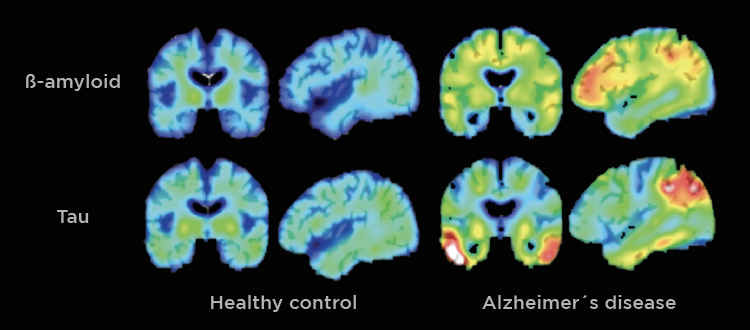
Fig. 1 – Using PET scans it is possible to visualize the deposition of β-amyloid and tau protein in the brains of Alzheimer’s patients.
What is the importance of sleep in the development of Alzheimer’s disease?
The effect of sleep deprivation (less than 7 hours of sleep per night) on the histological findings associated with Alzheimer’s disease is well documented in the scientific literature. Some of the mechanisms described are as follows:
- Sleep deprivation, especially in its slow wave phase (stages 3 and 4 of non-REM sleep) leads to increased β-amyloid protein deposition in the brain, particularly in the hippocampus – the area of the brain responsible for memory consolidation, among other functions. Some studies have shown that this effect can be observed after a single night of poor sleep.
- The activity of the enzymes involved in the phosphorylation of tau protein is also induced by the lack of sleep, promoting the formation of neurofibrillary tangles. Individuals who report sleeping fewer hours tend to have higher deposition of hyperphosphorylated tau protein.
- Increase in reactive oxygen species. These are products of cellular metabolism that have the ability to oxidize certain cellular structures, leading to damage. Sleep deprivation lowers the antioxidant capacity in the brain.
What is the glymphatic system?
There is a flow of cerebrospinal fluid in the brain that is particularly active during sleep, especially in its deeper stages. This system ensures neuron nutrition and the cleansing of their metabolic waste products. It has been shown in animals that sleep deprivation decreases the effectiveness of the glymphatic system. This interference may also explain the higher accumulation of β-amyloid when there is sleep deprivation.
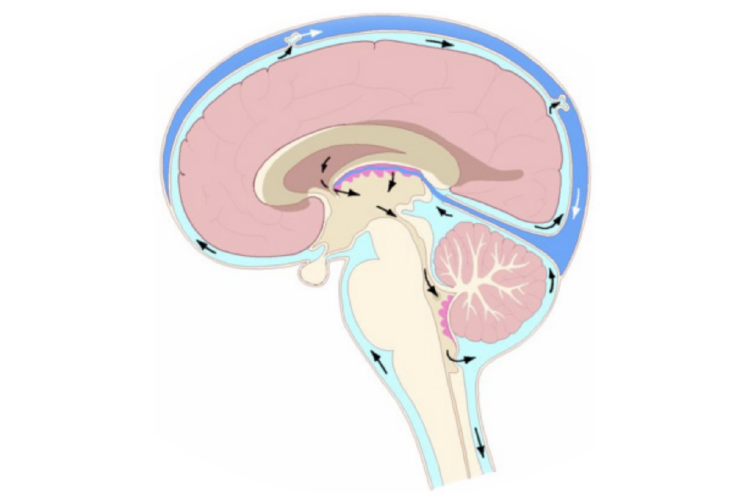
Fig. 2 – The cerebrospinal fluid flows through a specific circuit in the brain.
Who should be particularly aware of this association?
Sleep has so many benefits on human physiology that everyone should seek to optimize it. However, individuals carrying the apolipoprotein E gene ε4 allele should be particularly attentive to this relationship. The apolipoprotein E gene (ApoE) is responsible for coding this protein, which functions as the primary cholesterol transporter in the brain. There are three different alleles for the ApoE – ε2, ε3, and ε4 – that can be organized into six different genotypes (each individual inherits one allele from the father and another one from the mother) – 2/2, 2/3, 2/4, 3/3, 3/4 and 4/4. Although the precise mechanism is not fully understood, the risk of developing Alzheimer’s disease is increased in patients carrying ε4 alleles:
- ApoE 2/4 and 3/4 genotypes – risk increases 2-3 fold when compared to the genotype 3/3;
- ApoE 4/4 genotype – risk increases 12 fold when compared to the genotype 3/3.
It should be noted, however, that the presence of the ε4 allele is not deterministic for the development of Alzheimer’s disease. That is, one can have 1 or even 2 ε4 alleles and never develop this disease.
In an age when our brain is exposed to a wide range of stimuli unprecedented in the history of humanity, sleep deprivation is increasingly common. The ideal sleep duration varies with age, but should never be less than 7 hours per night. It is essential to spread this message so that we can reduce the risk of developing Alzheimer’s and other diseases.
References:
Ju, Yo-El S et al. Slow wave sleep disruption increases cerebrospinal fluid amyloid-β levels. Brain: a journal of neurology vol. 140,8 (2017): 2104-2111.
Ahmadian, Nahid et al. Tau Pathology of Alzheimer Disease: Possible Role of Sleep Deprivation. Basic and clinical neuroscience vol. 9,5 (2018): 307-316.
Shokri-Kojori, Ehsan et al. β-Amyloid accumulation in the human brain after one night of sleep deprivation. Proceedings of the National Academy of Sciences of the United States of America vol. 115,17 (2018): 4483-4488.
Wolfe, Cody M et al. The Role of APOE and TREM2 in Alzheimer’s Disease-Current Understanding and Perspectives. International journal of molecular sciences vol. 20,1 81. 26 Dec. 2018