18 . 09 . 2020
Chronic Stress - When the system reaches exhaustion
Any factor (physical or psychological) that causes tension in the body and a need for adaptation, is considered a stressor. There are forms of positive stress, such as exercise for example, and negative ones like sleep deprivation or relationship problems. Our body has a response system to stress, which is aimed at restoring balance. We’ll see what can happen if that system is overburdened.
The structures involved in the stress response system are the hypothalamus, the pituitary, and the adrenal glands. The hypothalamus and the pituitary are located in the brain and work together as the main regulators of hormonal synthesis in the body. The adrenals are two specialized glands, located above the kidneys, which produce the hormones and neurotransmitters responsible for promoting the physiological adaptations necessary to restore balance. This system is called the Hypothalamus-Pituitary-Adrenal (HPA) axis.
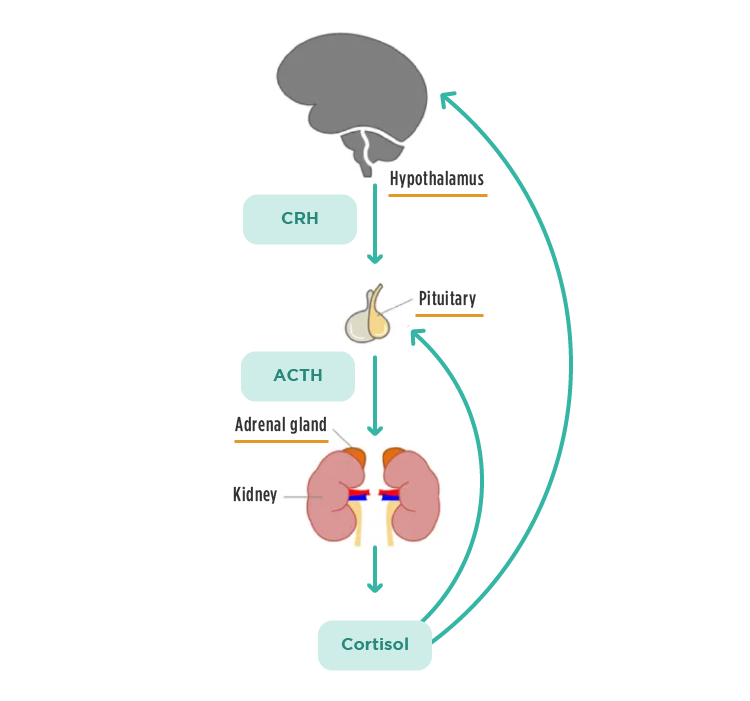
Fig.1 – HPA axis components and their communication.
What is the normal stress response?
When a stressor is perceived, the hypothalamus triggers a cascade of signals that leads to two types of response:
-
acute and short-term response – mediated by catecholamines (adrenaline and norepinephrine). These substances are released in seconds and cause an increase in heart rate and blood pressure, among other effects. It is this acute response that can save our lives, in the event of an accident and hemorrhage, for example.
-
delayed and long-term response – mediated by cortisol (steroid hormone produced in the adrenals). Cortisol prepares the body for a more prolonged response to stress, ensuring adequate glucose levels and suppressing the inflammatory response, for instance.
Ideally, stress is resolved and these responses are shut down.
How are cortisol levels controlled?
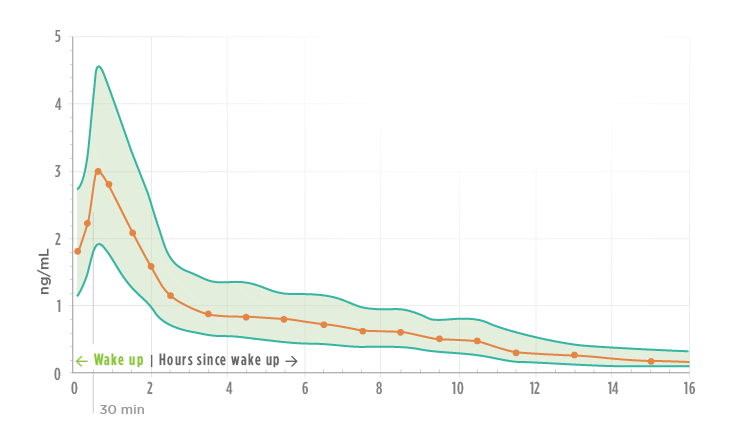
All substances fundamental to the functioning of the body are subject to strict control. Cortisol is no exception and follows a circadian rhythm. Cortisol secretion peaks about 30-45 minutes after waking up, as a result of hypothalamus stimulation by daylight. This cortisol morning peak is essential in order to feel the energy to start the day. Thereafter, cortisol levels decrease throughout the day and should be low at night to allow for sleep. When cortisol levels are very high, the hypothalamus detects it, through its sensors, and reduces the signaling for more production (negative feedback mechanism).
Fig. 2 – Average levels of salivary cortisol based on 15 different studies, with a total sample of 18,698 individuals (2).
What can happen when stress is chronic?
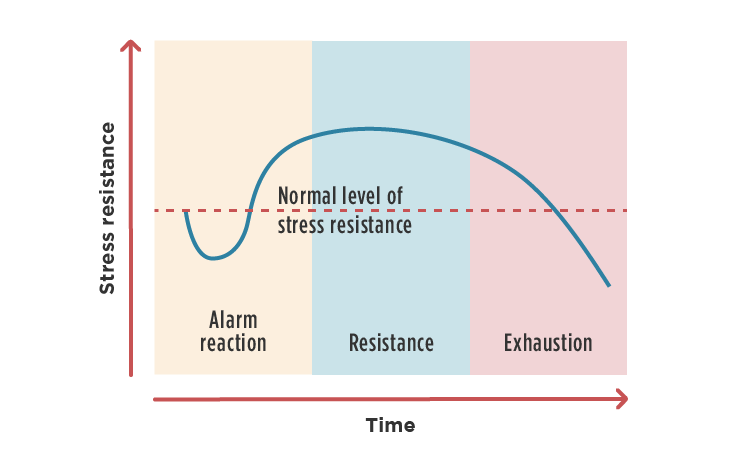
When there is no resolution of stress (whether psychological or physical), there will be constant pressure on the HPA axis for an increased cortisol output. This initially results in higher cortisol levels. However, over time, the body triggers a series of mechanisms to decrease cortisol levels and thus protect itself from its harmful effects, resulting in hypocortisolism. It is important to remember that cortisol is a catabolic hormone, which promotes the degradation of tissues such as muscle and bone, favoring other more important functions for survival. As such, continuously high levels of this hormone pose a metabolic risk.
Fig. 3 – The different stages of stress adaptation described by Hans Selye. The length of time it takes to reach exhaustion depends on the individual and his metabolic resilience.
What are the symptoms of hypocortisolism?
When the HPA axis is suppressed and cortisol levels decrease, the patient faces a situation of “burnout” or exhaustion. The most common symptoms are: extreme fatigue, muscle weakness, diffuse pain, depression, irritability and difficulty concentrating. It is important to distinguish this state of hypocortisolism from Addison’s disease, in which there is an autoimmune destruction of the adrenal gland and a consequent decrease in cortisol levels. In HPA dysfunction due to chronic stress, the problem does not lie in the adrenal glands themselves, but in the regulation mechanism, controlled by the hypothalamus and pituitary.
How can one avoid a burnout situation?
To answer this question, we will mention the four main triggers of HPA axis dysfunction, briefly suggesting what can be done in each of the categories to increase stress resilience.
1. Perceived stress – all stressful situations are perceived uniquely by different individuals. It is important to have tools to cope with stress and find solutions for adverse situations, if necessary with the help of specialized professionals.
2. Circadian rhythm – stable and consistent light/dark cycles are essential for proper body functioning, including maintaining healthy levels of cortisol. The ideal is 7-8 hours of continuous sleep, somewhere between 9 pm and 8 am.
3. Glycemic control – Cortisol plays an important role in regulating blood glucose levels. In situations of hypoglycemia, the production of cortisol is stimulated. On the other hand, metabolic dysfunction with high blood sugar and insulin levels will also lead to increased cortisol. Thus, we should follow a low sugar diet, rich in fiber, healthy fats, and protein, in order to stabilize blood glucose levels, and therefore avoid triggering the HPA axis.
4. Inflammation control – chronic inflammation promotes cortisol secretion (due to the anti-inflammatory effects of this hormone). It is important to screen for chronic and silent inflammation.
The HPA system is a fascinating evolution of nature that allows for an elegant control of the stress response. From a clinical point of view, many diseases originate from the overload, and consequent dysfunction, of this axis. Being aware of the typical symptoms of HPA dysfunction and using specific tests, the clinician can detect this problem in the early stages and help the patient to restore balance.
References:
- Guilliams, TG. The Role of Stress and the HPA Axis in Chronic Disease Management. Point Institute, 2015.
- Miller R, Stalder T, Jarczok M, et al. The CIRCORT database: Reference ranges and seasonal changes in diurnal salivary cortisol derived from a meta-dataset comprised of 15 field studies. Psychoneuroendocrinology. 2016;73:16-23.