
24 . 10 . 2019
The Dangers of Hormonal Contraceptives
Hormonal methods of contraception are very popular, and it is estimated that they are used by up to 40% of women of childbearing age. However, this use can cause multiple adverse effects, which will be explored in this article.
Hormonal contraception was introduced in the 1960s and has since gained popularity, being the preferred method. This type of medication ensures a continuous delivery of artificial steroid hormones, which through a negative feedback mechanism, suppresses the release of gonadotropins (messenger chemicals that stimulate the production of sex hormones by the ovaries), and prevents ovulation. Consequently, women stop having ovulatory cycles, and the monthly bleeding is only due to hormone withdrawal analogs, and should not be considered actual menstruation.
What are the hormonal methods of contraception?
There are several methods of hormonal contraception, not exclusively oral. The different categories are as follows:
- Combined pill – the most common method. It uses the combination of an artificial estrogen derivative (ethinyl estradiol) and a progestin (levonorgestrel, gestodene, drospirenone, etc.).
- Estrogen-free pill – composed solely of progestins, without the estrogen component. They have slightly lower contraceptive efficacy than the combined pill.
- Vaginal ring – combined non-oral method.
- Patch – ensures transdermal administration of an estrogen derivative and a progestin.
- Implant – long-term method (up to 3 years)
- IUD (intrauterine device) – local delivery of a progestin (levonorgestrel). It is a long-lasting method (usually 5 years).
What all these methods have in common is the administration of artificial sex hormone derivatives, whose chemical structure and function are not exactly similar to the estrogen and progesterone produced by women during a regular menstrual cycle.
What are the hormonal methods of contraception used for?
The main indication for these drugs is, in fact, contraception, and their effectiveness in this context is unquestionable.
However, there are several other clinical situations in which hormonal methods of contraception are used, such as the following:
- Acne – hormone analogs have a potent effect on reducing sebum production, which decreases acne.
- Dysmenorrhea (menstrual pain) and menorrhagia (heavy menstrual flow) – the pill relieves symptoms by preventing hormonal fluctuations in the menstrual cycle.
- Irregular periods – oral contraceptives are often used to “regulate” the period. However, this presumption is wrong, as the cycle will be suppressed and not regulated. As described above, monthly bleeding during the use of these medications does not correspond to true menstruation.
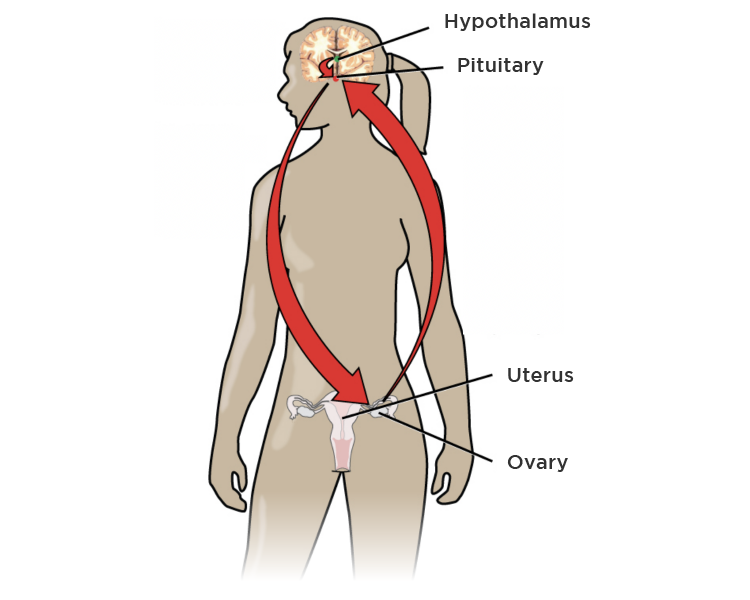
Fig. 1 – Bidirectional communication between the pituitary gland and the ovaries is interrupted by hormonal contraceptives, which results in the absence of endogenous sex hormone (estrogen and progesterone) production by the woman.
What, then, are the main risks of hormonal contraception?
Increased risk of venous thromboembolism
The incidence of venous thromboembolism (deep venous thrombosis and pulmonary thromboembolism) in women who do not use hormonal methods of contraception is about 1 in 10,000 women-years at age 20, rising to 5 in 10,000 women-years at 40 years old. In addition to hormonal contraception, factors such as family history, genetic mutations, smoking, and prolonged immobilization increase thromboembolic risk.
Combined pills increase the risk of thromboembolism by 3 to 6 times, depending on the progestin used. Non-oral combined methods (patch and vaginal ring) have a more pronounced effect, increasing the risk 6 to 8 times.
Non-estrogen methods (progestogen pill, IUD, and implant) do not lead to an increased risk of venous thromboembolism.
From a practical standpoint, the incidence of venous thromboembolism in a 20-year-old woman can increase from 1 in 10,000 women each year to 6 to 8, depending on the method of contraception used. In absolute numbers, this risk does not appear to be important, but if we add the presence of other risk factors, it can become significant.
Increased risk of arterial thromboembolism
The incidence of major arterial thrombotic phenomena (stroke and acute myocardial infarction) increases dramatically with age. In 10,000 women aged 45-49, 6.4 will have one stroke and 3.8 one myocardial infarction (MI) per year. Thus, for a woman over 35, arterial thromboembolic phenomena are more common than venous and are also more clinically severe.
The combined pill increases the risk of arterial thromboembolism by 1.5 to 2.2 times compared to women who do not take hormonal contraception. Non-oral combined methods (vaginal ring and patch) increase the risk between 2.5 and 3.2 times.
In turn, estrogen-free hormonal contraception (IUD and implant) methods do not confer any additional risk of arterial thromboembolism.
Increased risk of breast cancer
About 30% of cancers in women are in the breast, and only lung cancer is responsible for more deaths related to malignancy.
A Danish study published in the prestigious New England Journal of Medicine, in which 1.8 million women were followed for an average of 11 years, showed that women taking hormonal contraception had a 20% higher risk of getting breast cancer. This risk increased with the duration of contraceptive use and was 38% higher in women who used these drugs for more than 10 years.
In this study, the levonorgestrel IUD also led to a 20% increase in the incidence of breast cancer.
In absolute terms, the increase in cases of breast cancer diagnosed was 13 per 100,000 person-years, corresponding to 1 new diagnosis per 7690 women using hormonal contraception, per year.
Increased risk of depression
The effect of sex hormones on mood is well documented. Progestogens have a direct action on neurotransmitter receptors and levels such as GABA and serotonin.
Another study out of Denmark followed 1 million women over an average of 6.4 years, with 23,000 new cases of depression and 130,000 initial prescriptions of antidepressants. The risk of depression was 23% higher in women taking hormonal contraception. Particularly concerning in this study was the 70% higher risk of depression in the adolescent age group associated with the use of hormonal contraception.
Since depression is a very prevalent condition affecting about 5% of the female population, this increase in relative risk associated with hormonal contraception will have a more significant impact in absolute numbers.
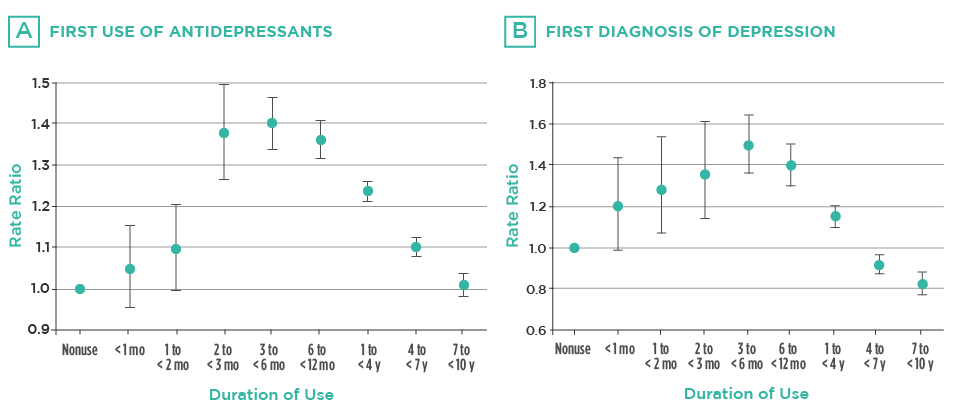
Fig. 2 – Graphs are representing the frequency of antidepressant use (A) and diagnoses of clinical depression (B) associated with hormonal contraceptive use. In both cases, there was a peak incidence at 3 to 6 months after the start of the medication.
Increased risk of suicide
In line with the association between hormonal contraception and the risk of depression, there is evidence that this category of drugs may also influence suicide attempts. This was the conclusion of a study, also Danish (in Denmark has an extensive database on the health of its inhabitants, which allows for in-depth population analysis), in which 475,000 women aged 15-33 were followed for an average of 8 years. Women using hormonal contraception were reported to have had twice as many suicide attempts and three times as more suicides.
This is very relevant, as the pill is often started in adolescence and can severely affect women’s psychological health.
Other adverse effects associated with hormonal contraception include decreased libido, a slight increase in blood pressure, hair loss, and possibly changes in bone mineralization. All of these factors must be taken into consideration when prescribing one of these drugs. Despite having great therapeutic utility, the contraceptive pill is not a harmless medication and should not be viewed as such.
References:
Lidegaard O, Nielsen LH, Skovlund CW, Løkkegaard E. Venous thrombosis in users of non-oral hormonal contraception: follow-up study, Denmark 2001-10. British Medical Journal. 2012;344:1-12.
Lidegaard O. Hormonal contraception, thrombosis and age. Expert Opinion on Drug Safety. 2014;13(10):1353-1360.
Mørch LS, Skovlund CW, Hannaford PC, Iversen L, Fielding S, Lidegaard Ø. Contemporary hormonal contraception and the risk of breast cancer. New England Journal of Medicine. 2017;377(23):2228-2239.
Skovlund CW, Mørch LS, Kessing LV, Lidegaard O. Association of hormonal contraception with depression. JAMA Psychiatry. 2016;73(11):1154-1162.
Skovlund CW, Mørch LS, Kessing LV, Lange T, Lidegaard J. Association of hormonal contraception with suicide attempts and suicides. American Journal of Psychiatry. 2018;175(4):336-342.